Categories
Change Password!
Reset Password!


HEART score consistently delivers stronger 30-day MACE prediction accuracy than the GRACE score, reshaping risk-stratification standards for acute chest pain in emergency care.
According to a new systematic review and meta-analysis, the HEART (history, electrocardiogram, age, risk factors, troponin) score offers better diagnostic accuracy than the GRACE (global registry of acute coronary events) score in forecasting 30-day major adverse cardiovascular events (MACE) among people presenting with acute chest pain in emergency departments (EDs).
Acute chest pain remains one of the most frequent and challenging ED presentations, and clinicians rely on rapid, evidence-based cardiovascular risk assessment to prevent missed diagnoses and unnecessary admissions. As risk-stratification tools continue to guide early decisions, HEART, and GRACE scores stand at the center of clinical protocols worldwide. However, uncertainty persists regarding which tool offers superior predictive precision for short-term MACE, including death, heart attack, and urgent revascularization.
To clarify this ongoing debate, the current study aimed to compare the diagnostic performance of the HEART and GRACE scores by evaluating their accuracy in predicting 30-day MACE among patients presenting with acute chest pain. Researchers carried out an extensive search of Web of Science, PubMed, Embase, Scopus, and the Cochrane Library from database. Eligible studies were required to be prospective cohorts that applied both the HEART and GRACE scores at the time of ED arrival.
Each study needed to report 30-day MACE outcomes and provide sufficient data to construct 2×2 diagnostic tables. With the help of bivariate random-effects model, pooling of diagnostic odds ratios, sensitivity, specificity, area under the curve (AUC), positive likelihood ratio, and negative likelihood ratio (NLR) was done. Statistical heterogeneity was evaluated using I² metrics, and predefined subgroup analyses explored the influence of geography, demographic characteristics, and scoring thresholds on diagnostic performance.
Across 19 qualifying studies encompassing 14,862 participants, the HEART score emerged as a superior tool for early risk rule-out:
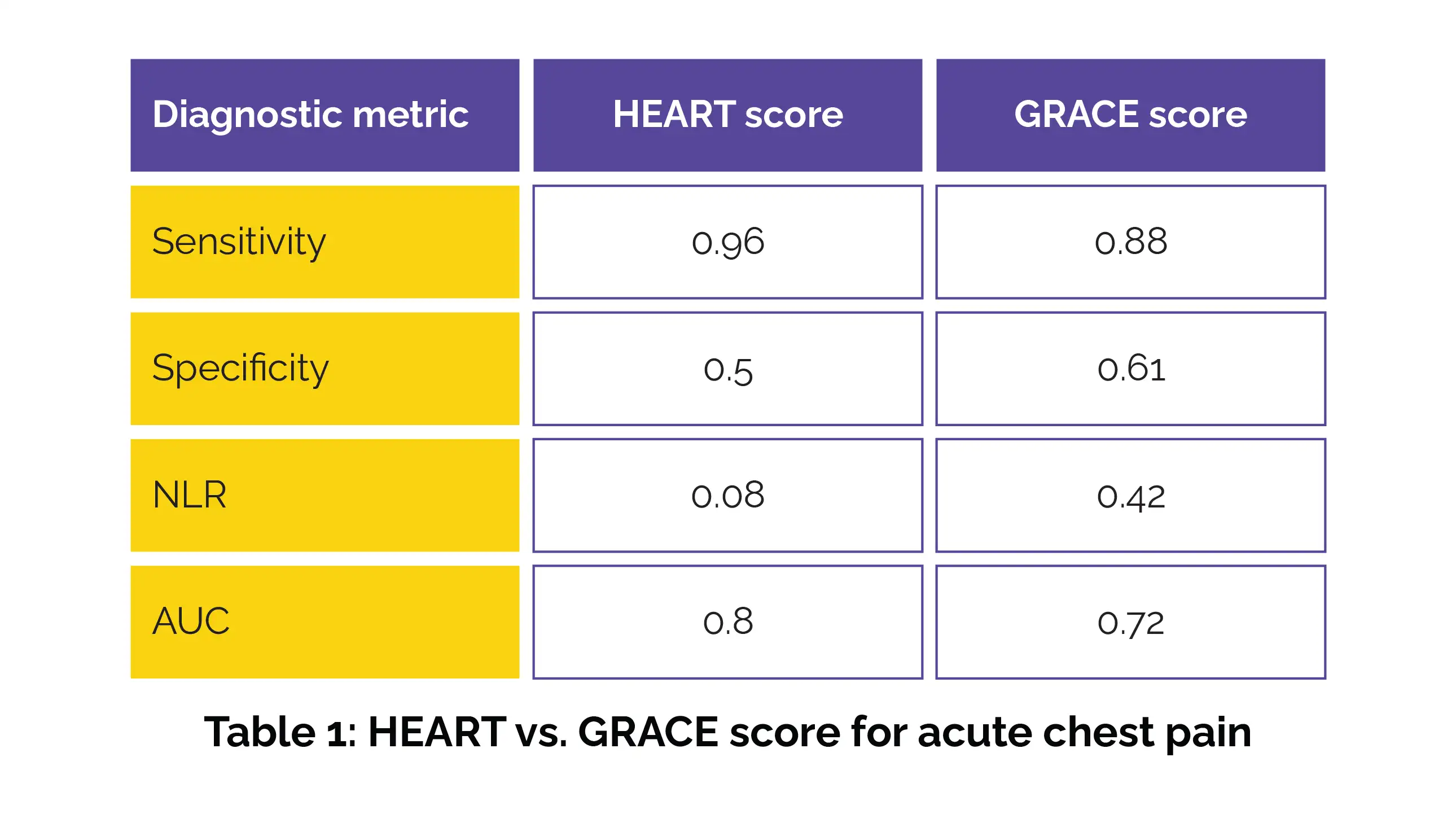
Subgroup analyses further revealed that HEART’s sensitivity advantage persisted across diverse regions and age groups, with the most pronounced performance gap observed in Eastern populations. The findings support prioritizing the HEART score in ED, especially where rapid decisions about discharge are needed.
Its high sensitivity and low NLR reduce the risk of missing patients who may develop heart attacks or other major cardiac events. Meanwhile, the GRACE score may remain valuable for determining escalation strategies, hospital admission, or cardiology referral for high-risk profiles. Researchers emphasize the need for future work on standardizing troponin assay thresholds and MACE definitions to support global implementation and clinical consistency.
Herz
HEART vs. GRACE scores for 30-day cardiovascular outcomes in acute chest pain
Peng-Fei Nie MM et al.
Comments (0)