Категории
Сменить пароль!
Сброс пароля!





Пожалуйста, подтвердите, что вы являетесь специалистом здравоохранения – пройдите регистрацию, чтобы получить полный доступ ко всем материалам!
специалистов здравоохранения
уже с нами!
научных статей,
исследования, рекомендации
записей видеолекций
и докладов

Действия и статус в суде и при общении с надзорными органами


Используйте в ежедневной практике для повышения точности диагностики



Пациенты не хотят терпеть боль: как меняется парад...
Если раньше боль воспринималась как естественный спутник болезни или лечения, сегодня она всё чаще рассматривается как самостоятельное клиническо...


Кратковременный приём НПВП: безопасно или рискован...
Использование НПВП может считаться относительно безопасным, если их назначать в наиболее эффективной дозе и на минимальный срок — не более...
1 мин

Маски ГЭРБ у детей: диагностические трудности и кл...
Частота выявления рефлюкс-эзофагита у детей с заболеваниями пищеварительной системы — от 8,7% до 17% [1]. Распространенность ГЭРБ в детском...
1 мин

Мультиморбидность: когда все болезни — главные
Около трети взрослого населения и более половины пациентов с хроническими заболеваниями страдают мультиморбидностью [1]. С возрастом риск значите...
1 мин

Антигистаминные препараты при беременности и лакта...
От 27% до 93% женщин принимают по крайней мере один лекарственный препарат во время беременности [1]. Часто лекарства назначаются по жизненным по...
1 мин

Коллаген как вклад в долголетие
В условиях демографических вызовов геропротекция становится ключевым направлением медицины. Особое внимание уделяется сохранению скелетно-мышечно...
1 мин

Антигистаминные препараты в клинических рекомендац...
Клинические рекомендации (КР) не могут выступать предметом государственного контроля качества и безопасности медицинской деятельности и не имеют...
2 мин

Локомотивный синдром: пути диагностики и терапии
Старение населения стало глобальным процессом: доля людей старше 65 лет выросла с 6% в 1990 году до 9% в 2019 году и, по прогнозам, достигнет 16%...
3 мин

Эволюция эндоскопии: от первых экспериментов до со...
Современная гастроэнтерология немыслима без эндоскопии, но путь к ней был долгим, тернистым и болезненным… для пациентов. Как же развивала...
2 мин

Пациент 2025: как изменились ожидания за последние...
Как общаться с поколением Google? 41% пациентов после приема у врача сразу пойдут перепроверять ваш диагноз в интернете. Эта цифра – не пр...
1 мин

Особенности аллергии в конце лета
R1368282-18072025-HCP
1 мин

Замена лекарства: врач проиграл суд пациенту
Житель Новосибирска обратился в суд, усмотрев несоответствие предоставленного ему лекарственного средства нормативам, принятым при лечении по ОМС...
1 мин

Уголовное преследование медиков не сбавляет оборот...
Вопрос уголовной ответственности медиков за профессиональные ошибки остаётся остро актуальным. Юристы, специализирующиеся на защите врачей, сообщ...
1 мин

ХБП как фактор риска потери зубов
Влияние хронической болезни почек на состояние полости рта — тема, привлекающая всё больше внимания. Новое исследование, опубликованное в ж...
1 мин

Безникотиновый вейп: новые данные о влиянии на раз...
Учёные пристально изучили влияние на беременных мышей двух популярных основ для вейп-жидкостей без никотина: 30/70 (пропиленгликоль/растительный...
1 мин

Замена лекарства: врач проиграл суд пациенту
Житель Новосибирска обратился в суд, усмотрев несоответствие предоставленного ему лекарственного средства нормативам, принятым при лечении по ОМС...


Уголовное преследование медиков не сбавляет оборот...
Вопрос уголовной ответственности медиков за профессиональные ошибки остаётся остро актуальным. Юристы, специализирующиеся на защите врачей, сообщ...
1 мин

ХБП как фактор риска потери зубов
Влияние хронической болезни почек на состояние полости рта — тема, привлекающая всё больше внимания. Новое исследование, опубликованное в ж...
1 мин

Безникотиновый вейп: новые данные о влиянии на раз...
Учёные пристально изучили влияние на беременных мышей двух популярных основ для вейп-жидкостей без никотина: 30/70 (пропиленгликоль/растительный...
1 мин

Лидер по безопасности среди ПОАК при мерцательной...
Несмотря на полуторадесятилетний опыт использования прямых оральных антикоагулянтов (ПОАК) у людей с фибрилляцией предсердий (ФП), врачи не прекр...
1 мин

Как ранний приём пищи помогает контролировать вес?
Учёные выяснили, что для поддержания здорового веса важен не только состав рациона, но и время его употребления. Команда исследователей из Испани...
1 мин

Искусственный интеллект в медицине требует правовы...
Проблема регулирования ИИ в медицине 21 июля в Госдуме состоялось ключевое обсуждение этой темы в рамках круглого стола "Развитие здравоохр...
1 мин

Фото глазного дна предскажет риск инфаркта
Международная группа учёных из Университета Данди представила революционную систему анализа снимков глазного дна, основанную на искусственном инт...
1 мин

Метформин снижает риск выкидышей при СПКЯ: новые д...
Последние исследования подтверждают положительное воздействие метформина на течение беременности у пациенток с СПКЯ — распространённым эндо...
1 мин

Коморбидность — путь к депрессии: сочетание болезн...
Влияние сопутствующих заболеваний на риск депрессивных состояний стало предметом изучения в статье, опубликованной в журнале Communications Medic...
1 мин

Синдром задержки роста плода: Предикция и Превенци...
Уважаемые коллеги! Приглашаем вас на вебинар «Синдром задержки роста плода: Предикция и Превенция». В рамках цикла научно-образовате...
60 мин

Ответственность врача, действия и статус в суде и...
Уважаемые коллеги! Приглашаем вас на вебинар «Ответственность врача: действия и статус в суде и при общении с надзорными органами&raq...
60 мин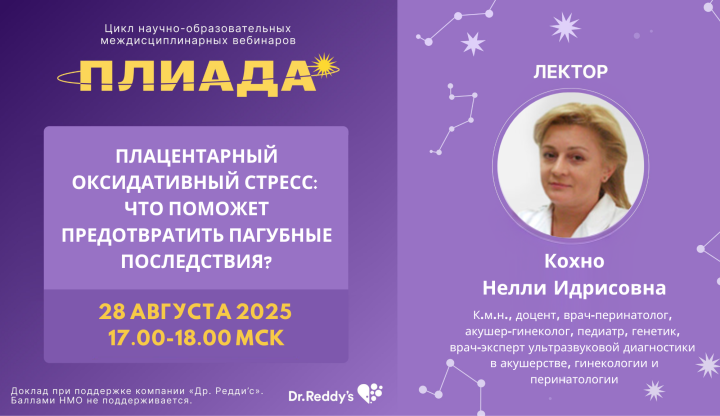
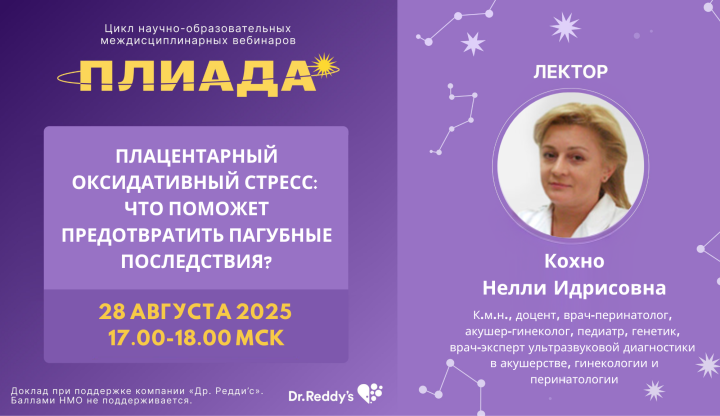
Плацентарный оксидативный стресс: Что поможет пред...
Уважаемые коллеги! Приглашаем вас на вебинар «Плацентарный оксидативный стресс: Что поможет предотвратить пагубные последствия?». В...
60 мин

Межрегиональная научно-практическая с международны...
Приглашаем Вас принять участие в Межрегиональной научно-практической конференции с международным участием «Все, или почти все о панкре...
1080 мин

Плацентарная недостаточность как фактор риска осло...
Уважаемые коллеги! Приглашаем вас на вебинар «Плацентарная недостаточность как фактор риска осложнений беременности. Современные практическ...
60 мин
Аллергический ринит: Старая проблема, новые решени...
Уважаемые коллеги! Приглашаем вас на вебинар «Аллергический ринит: Старая проблема, новые решения». В рамках цикла научно-образовате...
60 мин
Влияние оксидативного стресса на развитие беременн...
Уважаемые коллеги! Приглашаем вас на вебинар «Влияние оксидативного стресса на развитие беременности». В рамках цикла научно-образов...
60 мин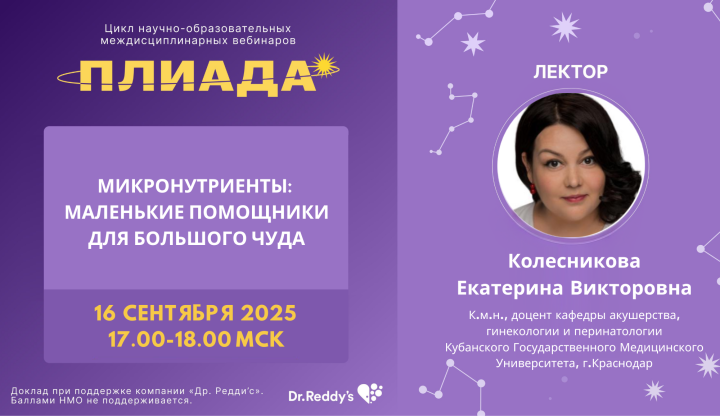
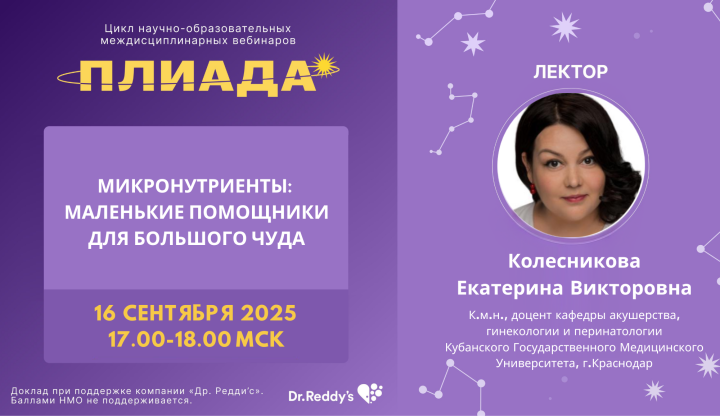
Микронутриенты: Маленькие помощники для большого ч...
Уважаемые коллеги! Приглашаем вас на вебинар «Микронутриенты: Маленькие помощники для большого чуда». В рамках цикла научно-образова...
60 мин

Динамика отоскопической картины при остром среднем...
Уважаемые коллеги! Приглашаем вас на вебинар «Динамика отоскопической картины при остром среднем отите у детей: Разбор клинических случаев&...
60 мин

Х Юбилейная Международная медицинская выставка «Зд...
Уважаемые коллеги! Приглашаем вас на Х Юбилейную Международную медицинскую выставку «Здравоохранение. Крым 2025» при поддержке Минист...
1110 минМы используем cookie файлы, чтобы сайт работал для Вас быстрее и эффективнее. Продолжая использовать сайт, вы соглашаетеесь на обработку файлов cookie в соответствии с Политикой [ссылка на Cookie политику].