Categories
Change Password!
Reset Password!


Acute pancreatitis is an inflammatory state of the pancreas that ranges from 4.9 to 35 per 100,000 population annually, and about 15 to 25% of people suffering from acute pancreatitis have the possibility to get severe acute pancreatitis.
Ketorolac may enhance feeding outcomes with no need for tube feeding and reduce the length of hospitalization in people with predicted severe acute pancreatitis.
Acute pancreatitis is an inflammatory state of the pancreas that ranges from 4.9 to 35 per 100,000 population annually, and about 15 to 25% of people suffering from acute pancreatitis have the possibility to get severe acute pancreatitis. Activated pancreatic enzymes and cytokines are discharged into the circulation by the damaged pancreas. This can impair the pancreas and also elicit systemic inflammatory response syndrome (SIRS) in an individual.
The SIRS is balanced by a compensated anti-inflammatory response syndrome that results in recovery. Severe organ failure may occur due to an imbalance between anti-inflammatory and inflammatory responses. Research has revealed that administration of interleukin 10 (IL-10) can lead to early suppression of proinflammatory cytokine activity. This anti-inflammatory cytokine has the ability to lower severity of experimental pancreatitis in animals and also avoid post endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis in human beings.
Ketorolac possessing anti-inflammatory, analgesic and antipyretic effects, suppresses cyclooxygenase-1 and 2 enzymes. This leads to a reduction of prostaglandin precursors formation. Suppressing neutrophil aggregation/activation, reducing proinflammatory cytokine levels, altering lymphocyte activity, and curbing chemotaxis are amidst other mechanisms suggested for ketorolac that impart anti-inflammatory effects.
The severity of pancreatitis is related to the extent of inflammation; hence, the early decrease in inflammation with ketorolac usage can reduce the outcomes of morbidity and development of organ failure in acute pancreatitis patients. Late feeding because of pain in acute pancreatitis and unused gastrointestinal tract, breaks tight junction of enterocytes and additionally elevates the chance of organ dysfunction and inflammation in people having acute pancreatitis. In the current investigation, it was assumed that the ketorolac when given to the patients, could decrease the organ failure and inflammation of pancreatitis, decrease the length of hospitalization, manage pain and food intolerance, and promote earlier feeding.
RATIONALE BEHIND RESEARCH
No study has evaluated the influence of ketorolac injection on clinical outcomes and feeding in individuals having predicted severe acute pancreatitis. Therefore, this study was performed.
OBJECTIVE
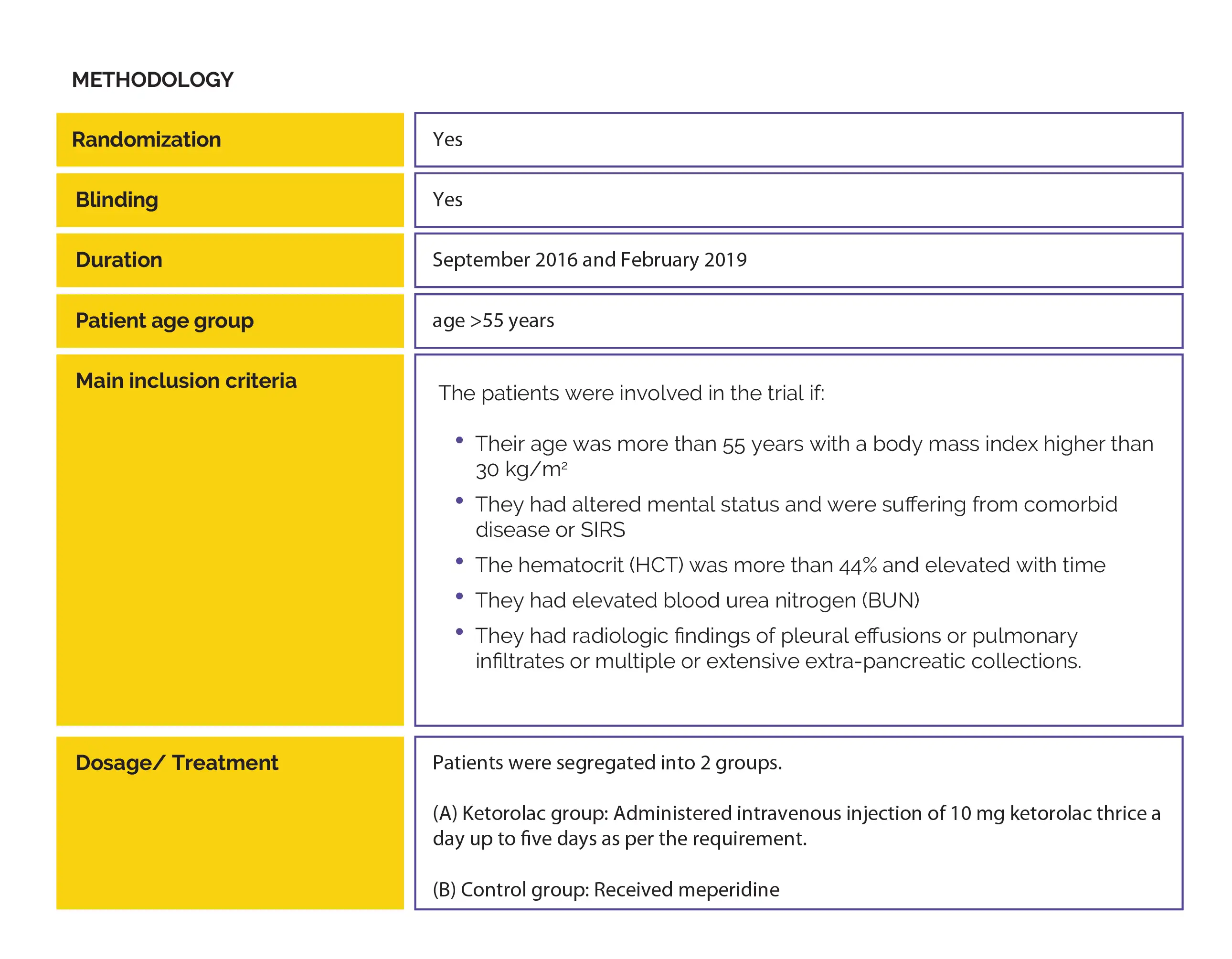
A randomized controlled clinical trial sought to examine the effectiveness of ketorolac for the management of predicted severe acute pancreatitis.
Study outcomes

Outcomes
Baseline: There were no vital differences reported at baseline.
Study outcomes
This trial aimed to explore ketorolac's efficacy in people with predicted severe acute pancreatitis.
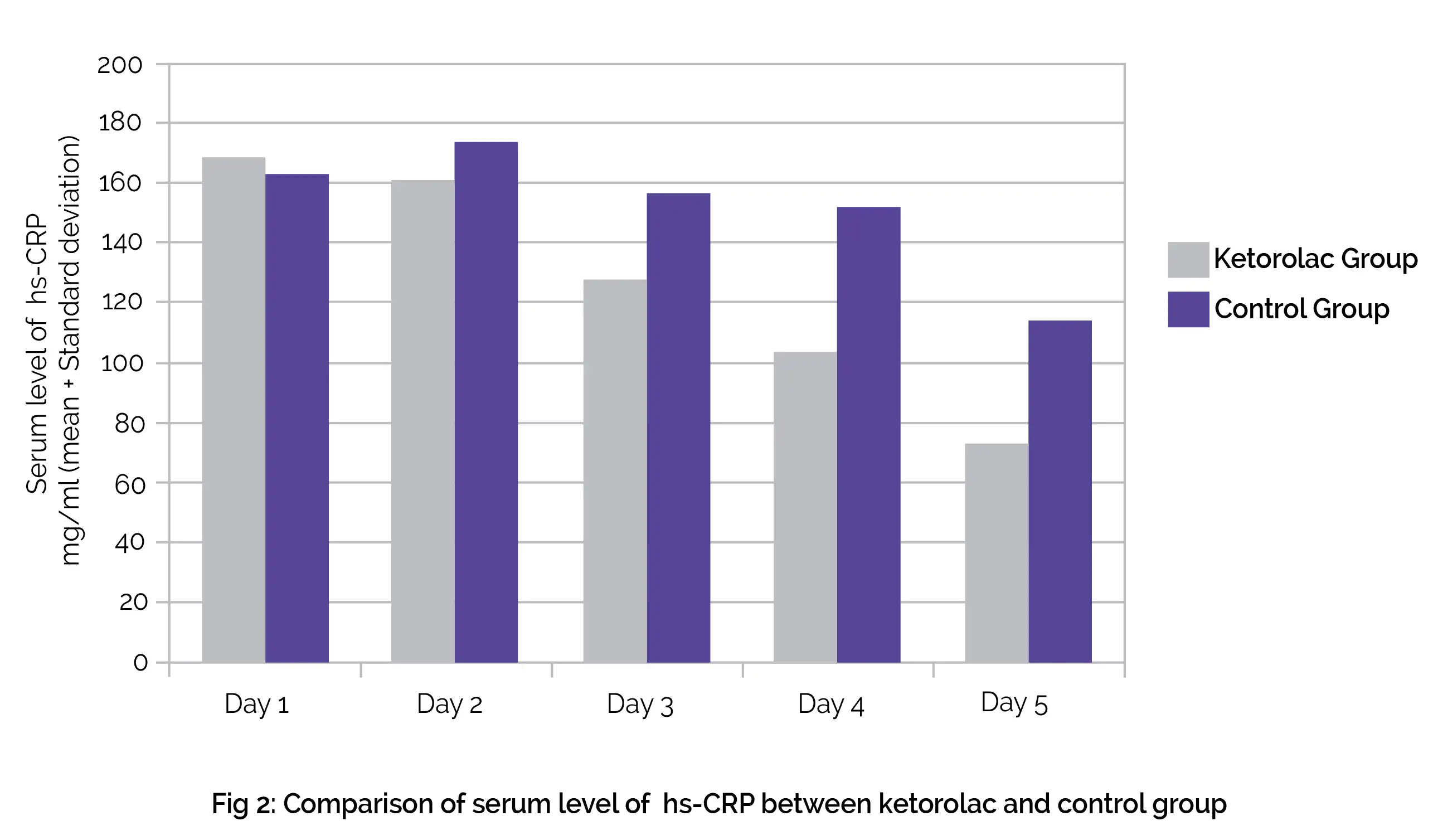
Serum hs-CRP level was reported to decrease faster in people who were administered ketorolac, and these people were discharged earlier. Feeding was started earlier in the ketorolac group than the control group, no requirement for tubing was there, and better food tolerance was seen with ketorolac use. No difference in mortality and organ failure was seen.
The severity of pancreatitis is associated with the extent of inflammation in acute pancreatitis people. Chemo-attraction of leukocytes takes place in acute pancreatitis pathogenesis. Moreover, proteolytic and lipolytic enzymes, reactive oxygen metabolites, proinflammatory cytokines and arachidonic acid metabolites are liberated by activated macrophages/granulocytes. Pancreatic damage is triggered by these factors.
The level of CRP elevates in the liver concerning pancreatitis severity, and in response to interleukin-6 and interleukin-1. CRP, a marker of inflammation, can predict prognosis and complications in acute pancreatitis patients. Ketorolac (NSAID with anti-inflammatory and analgesic characteristics) inhibits cyclooxygenase-1 and 2 enzymes. This, in turn, prevents the production of prostaglandin precursors.
According to the findings of a randomized controlled trial carried out by Vege et al., the usage of pentoxifillyne (tumor necrosis factor [TNF] inhibitor) was related to reduced hospitalization time and minimized ICU stay in people suffering from predicted severe acute pancreatitis. The level of serum TNF, CRP, interleukin-6, and interleukin-1 were considerably reduced in the pentoxifillyne group; the decrease was not statistically considerable that might be due to small sample size.
For post-ERCP pancreatitis, few studies have analyzed preventive effects of diclofenac or rectal indomethacin, with a meta-analysis that confirmed their protective effect. Another meta-analysis exhibited that in high-risk people, administration of rectal indomethacin before ERCP was efficient to prevent post-ERCP pancreatitis. Rectal NSAIDs inhibited phospholipase A2 activity in acute pancreatitis, thereby regulating proinflammatory mediators.
The early feeding showed an influence on mitigating the inflammatory response by itself. The traditional approach of feeding a person with parenteral nutrition in acute pancreatitis and putting the pancreas at rest has been altered. The findings of a meta-analysis depicted that in severe acute pancreatitis, the use of the gastrointestinal tract to feed is associated with reduced mortality, organ failure, surgical intervention rate, and infectious complications when compared to parenteral nutrition.
As suggested by the American Society of enteral and parenteral nutrition, the enteral feeding must be commenced at a trophic rate in individuals intolerant of oral feeding. People having moderate to severe acute pancreatitis deny oral feeding due to abdominal pain, vomiting and nausea secondary to abdominal distention and gastric stasis following inflammation of the pancreas. In early tube feeding, food intolerance is also witnessed. The severity of intolerance rises and feeding becomes more problematic as a result of aggravation in pancreatic inflammation.
The outcomes of this study exhibited that all subjects in the ketorolac group were able to tolerate oral feeding with no need for tube feeding. Notably, the time span for feeding initiation was less in the ketorolac group, possibly pertaining to the potent anti-inflammatory characteristics of ketorolac and its analgesic effects. The frequency of NPO was reduced in patients administered with ketorolac along with lesser days of hospitalization.
The intestinal permeability ranges from mild to severe forms in acute pancreatic. It has been depicted that the integrity of the intestine is maintained using the gastrointestinal tract for feeding and it lowers the plasma endotoxin levels and minimizes the translocation of bacteria in mesenteric lymph nodes too. The intestinal microbiota is changed by starvation. The proinflammatory patterns are also triggered by starvation.
It was reported that in acute pancreatitis people, failure to initiate tube feeding for greater than 3- 4 days after admission elicits the chance of deteriorated nutrition status and occurrence of SIRS, infection and organ failure. On the basis of these recommendations, tube feeding was initiated on day 5 in all people unable to be fed. Notably, 21% of people were on tube feeding in the control group.
Oral feeding was initiated before the fifth day of admission with no requirement for tube feeding in all patients who were given ketorolac. Earlier feeding and lowered inflammation were seen in the ketorolac group. This can be the reason for reduced ICU stays, fewer organ failures, and the prevented advancement of predicted severe acute pancreatitis to serious forms.
For people suffering from predicted severe acute pancreatitis, administration of ketorolac is valuable as it may shorten the length of hospital stay, improve feeding outcomes with no requirement for tube feeding, and thus result in higher nutrition delivery.
Clinical Medicine and Research
Ketorolac and Predicted Severe Acute Pancreatitis: A Randomized, Controlled Clinical Trial
Zahra Vahdat Shariatpanahi et al.
Comments (0)