Categories
Change Password!
Reset Password!


The field of medicine has witnessed incredible advancements in recent years, leading to a shift from a one-size-fits-all approach to a more personalized and precise approach. [1] Healthcare professionals have strived to enhance their practices and ensure greater effectiveness and safety for their patients, building upon the achievements of previous generations. With the aid of electronic health records, supercomputing, big data analytics, and genetic testing (all ingredients needed to engage in what is quickly becoming truly precise and personalized medicine), scientists and physicians are now able to take this mission far. [2]
Precision medicine and personalized medicine are two terms that have gained prominence in this paradigm shift. Conventionally, medicine has followed a one-size-fits-all approach, where treatments are designed based on population averages. But, this strategy fails to account for the inherent differences between individuals. The approach of precision and personalized medicine recognizes that each person's genetic and biological composition is distinct, and therefore, their response to treatment can vary significantly. [3]
These approaches take into account an individual's unique genetic makeup, environmental, and lifestyle factors to offer tailored medical interventions. [4] Personalized medicine encompasses an approach to patient care that takes into account not only their genetic characteristics but also factors such as preferences, beliefs, attitudes, knowledge, and social context. On the other hand, precision medicine refers to the healthcare delivery model that heavily relies on data, analytics, and information to yield targeted and accurate treatments. [5]
By leveraging the patient's genetic characteristics, personalized medicine holds the potential to provide tailored drugs at precise dosages and optimal timings, thus boosting efficiency in medical practice and reducing healthcare expenses. [6] Precision medicine adopts a more nuanced strategy, taking both genotypic and phenotypic differences into account, in order to create a therapy or preventative method that may be used to benefit both populations and individuals. [7]
The progress in precision medicine is leading to tangible advantages, including the ability to detect illnesses at an early stage and create personalized treatment plans. The personalized care made possible by precision medicine relies on various data collection and analytics technologies. Notably, the integration of high-throughput genotyping with the widespread use of electronic health records presents an unparalleled opportunity for scientists to extract novel phenotypes from real-world clinical and biomarker data.
These phenotypes, when combined with electronic health records knowledge, have the potential to validate the necessity for additional treatments or enhance the accuracy of diagnosing disease variants. [8] This article explores the concept of precision and personalized medicine and its potential to unlock a new era in healthcare.
Precision Medicine vs. Personalized Medicine: What Is the Difference?
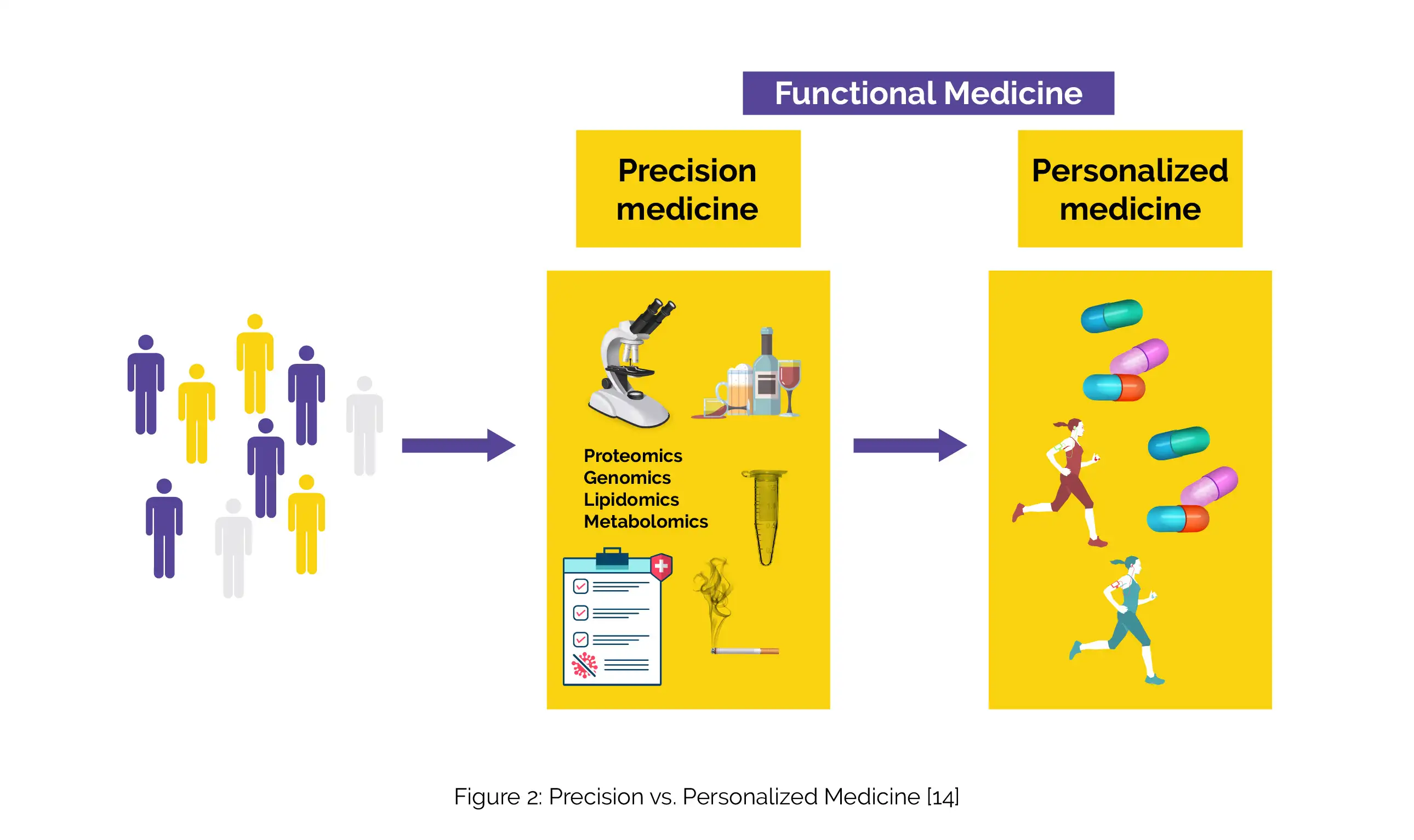
A novel era of "personalized" or "precision" medicine that considers individual genetics and other sources of variability in treatment and prevention of illness, has been ushered in by advances in genomics and other "omic" technology. [9] The National Research Council claims that "personalized medicine" is a more ancient phrase with a connotation more similar to "precision medicine." [10] Precision medicine and personalized medicine are usually used interchangeably. But, there is a little difference between the two concepts.
(A) Precision Medicine: Precision medicine refers to an approach that aims to tailor medical treatments and interventions to individual patients based on their specific characteristics, including their genetic makeup, environmental factors, lifestyle, and other relevant data. It emphasizes the customization of healthcare to optimize effectiveness and diminish adverse effects.
Its goal is to offer the correct treatment to the patient at the appropriate time. Precision medicine relies on advancements in technologies such as genomics, proteomics, and other "-omics" fields, as well as bioinformatics and data analysis, to identify molecular and genetic markers that can help anticipate disease risk, diagnose conditions, and guide treatment decisions (Figure 1).
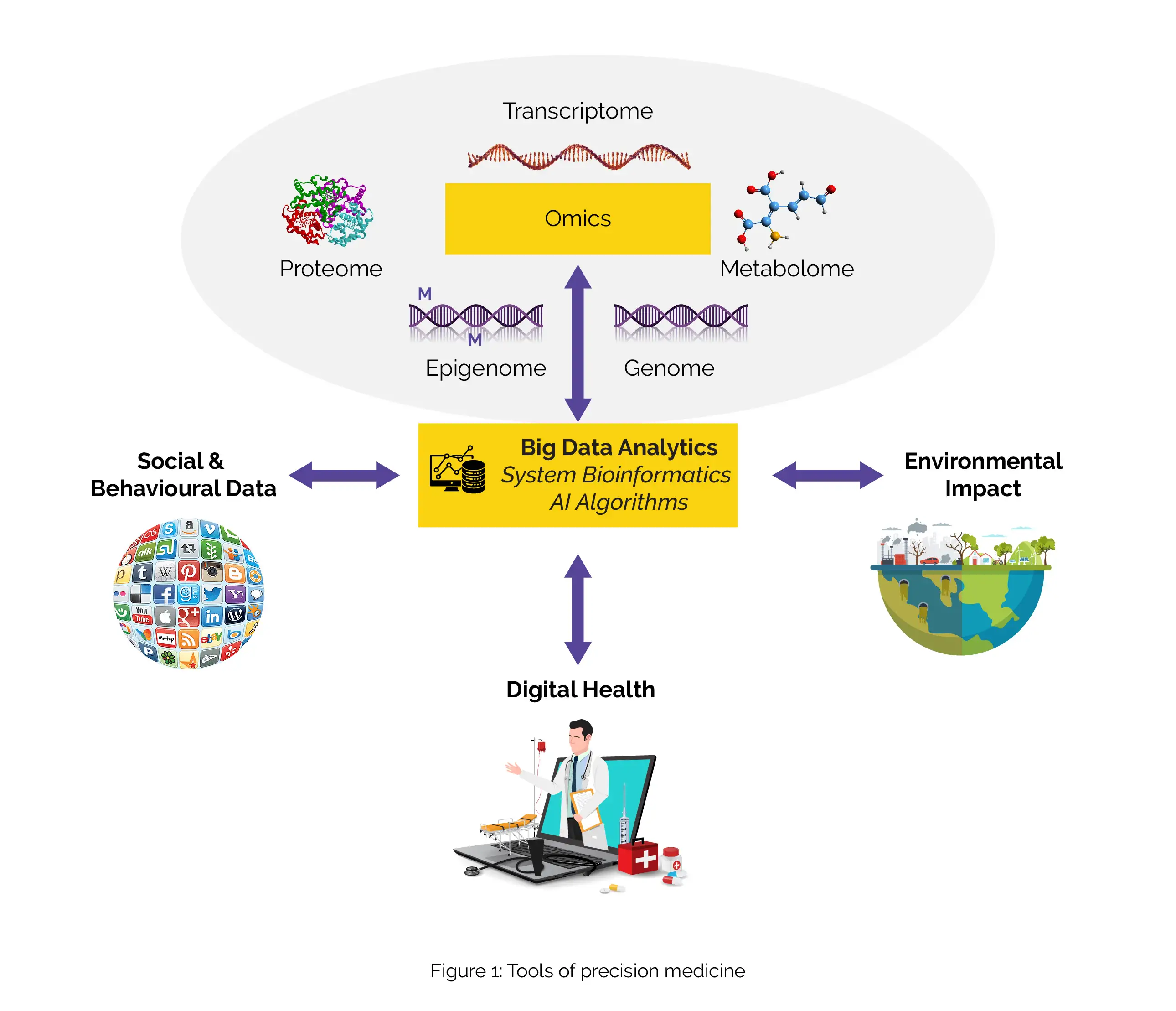
By understanding the unique genetic and molecular profiles of patients, precision medicine enables more targeted and tailored interventions.
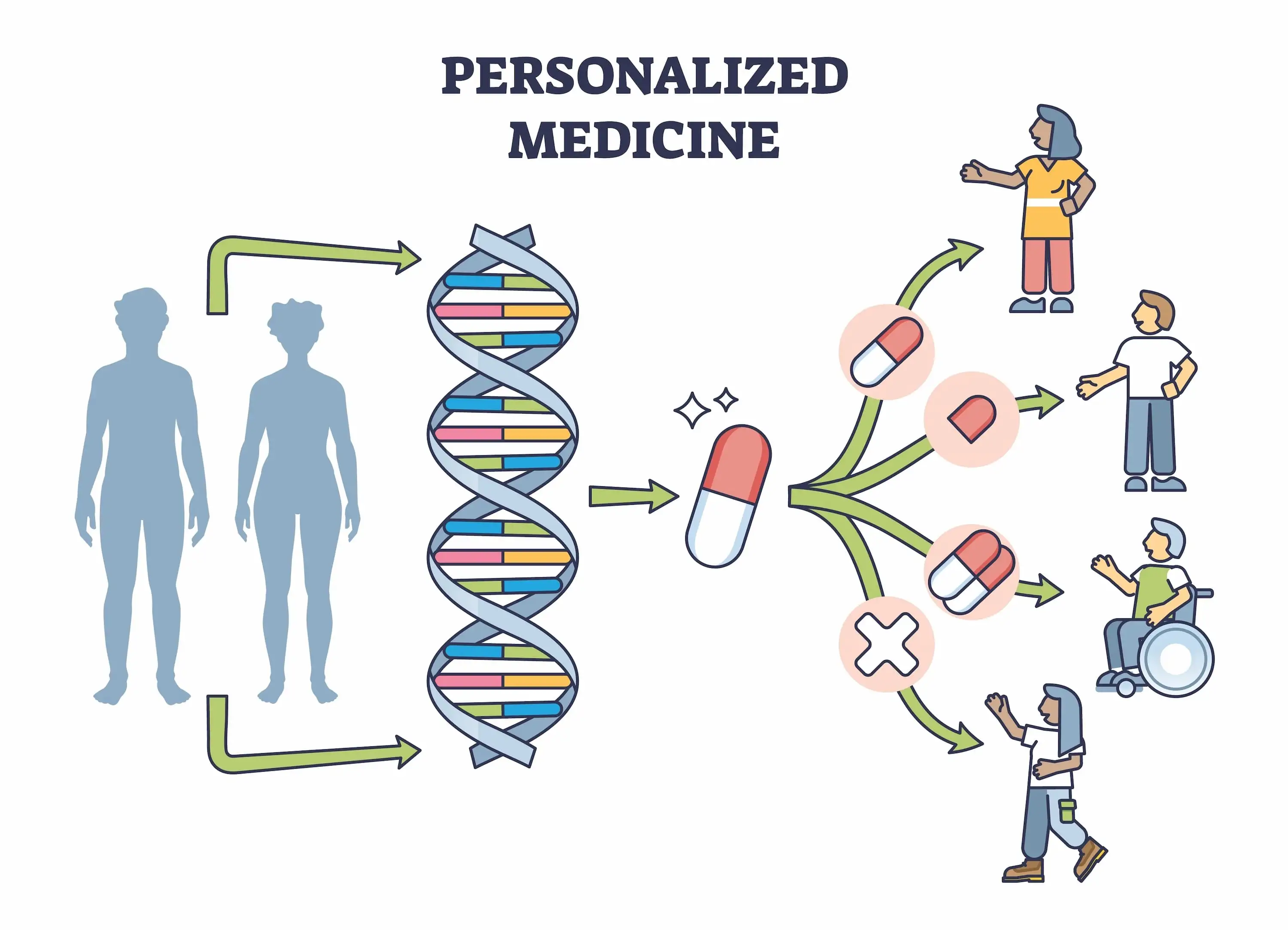
(B) Personalized Medicine: Personalized medicine, on the other hand, takes a broader approach by considering not only the individual patient's biological characteristics but also their personal preferences, values, and circumstances. It recognizes that healthcare decisions should be made in partnership with patients, taking into account their unique needs and circumstances.
In addition to biological factors, personalized medicine incorporates social, psychological, and behavioral aspects to create a comprehensive healthcare plan that aligns with the patient's goals and values. It focuses on patient-centered care, patient empowerment, and shared decision-making. While precision medicine focuses primarily on the biological and molecular aspects of healthcare customization, personalized medicine extends the concept to encompass a more holistic view of the patient and their healthcare journey.
In summary, precision medicine emphasizes the use of molecular and genetic information to guide treatment decisions, whereas personalized medicine takes into account a broader range of factors, including the patient's preferences and values, to create an individualized healthcare plan (Figure 2).[11-13]
Role of Precision and Personalized Medicine in Revolutionizing Healthcare
The remarkable advancements in genomics research over the past few decades have sparked high hopes for its profound influence on the field of biomedicine. Consequently, there has been a substantial rise in research funding directed towards personalized or precision medicine, which strives to tailor medical approaches to individual patients. This approach relies on genetic testing, biomarker identification, and the creation of targeted medications, all with the aim of offering customized medical care.
In recent years, precision and personalized medicine have emerged as transformative approaches in revolutionizing healthcare. [6] Let's explore how precision and personalized health approaches can enhance disease prediction, prevention, and treatment for individuals and their families.
(A) PREDICTION AND PREVENTION
1. Understanding your family health history is crucial
Knowing the chronic diseases prevalent among your family members, such as diabetes, heart disease, high blood pressure, or cancer, can provide insights into your own risk factors. Sharing this information with your doctor enables proactive steps to prevent diseases or detect them early. In certain cases, your doctor might recommend genetic counselling and testing to assess your susceptibility to diseases running in your family.
2. Leveraging mobile health applications
Utilizing smart devices and mobile health applications allows you to track vital health information like nutrition, physical activity, and blood pressure. Real-time measurements help you monitor progress and receive alerts indicating any changes that might necessitate medical attention. However, it is important to note that these devices should not replace regular medical checkups but serve as complementary tools.
3. Harnessing the power of social media
Public health researchers are exploring the potential of social media in tracking disease outbreaks. By monitoring posts that self-report symptoms, valuable information can be gathered to identify and analyze trends. Health departments can effectively communicate important health information to a larger audience through social media platforms.
4. Uncovering infectious disease outbreaks
Genome sequencing plays a vital role in identifying the specific pathogens causing illnesses by providing their DNA fingerprints. This information enables doctors and public health officials to pinpoint the sources of infections and choose the most appropriate treatment strategies. Accurate tracking of pathogens becomes feasible, facilitating effective disease control measures.
5. Preventing complications through early intervention
Newborn screening is a critical process that involves testing infants for specific medical conditions shortly post-birth. It includes blood tests, screenings for hearing loss, and evaluations for heart defects. Early identification of these conditions allows for prompt treatment, reducing the risk of disability or death.
6. Preventing diseases in individuals with genetic predispositions
Certain individuals have inherited conditions that increase their susceptibility to specific diseases. For example, individuals with BRCA1 or BRCA2 gene mutations have a higher risk of breast or ovarian cancer, while those with Lynch syndrome are prone to colorectal and other cancers. Recognizing these conditions empowers individuals to take preventive measures, such as earlier or more frequent screenings, medication usage, or even surgical interventions, to reduce their disease risks.
(B) TREATMENT AND MANAGEMENT
1. Biomarker testing aids doctors in selecting the most effective treatment
Biomarker testing, also known as tumor profiling or tumor genetic testing, examines genetic or other alterations in solid tumors and blood cancers. By identifying these changes, doctors can determine the most suitable treatment option. Even if two individuals have the same cancer type, their treatments may differ. Biomarker testing can also predict the likelihood of cancer recurrence, assisting individuals in deciding whether to pursue treatments like chemotherapy or radiation.
2. Pharmacogenomics assists doctors in prescribing the most suitable drug and dosage
Your response to medication is influenced by various factors, including your DNA. Some individuals may benefit from a particular drug, while others may experience poor response or severe side effects. Pharmacogenomics studies how your DNA affects drug response and helps doctors select a drug and dosage that is safe and likely to be effective for you.
3. Continuous glucose monitoring systems enhance insulin dosage
Regular blood sugar monitoring is crucial for effectively managing diabetes with insulin. Continuous glucose monitoring systems utilize sensors attached to the arm or stomach to provide persistent monitoring of blood sugar levels. Their usage improves insulin dosage, prevents complications, and enables users to share their results with healthcare providers.
4. Mobile devices facilitate healthy living and improve chronic disease management
Personal devices can track behaviors such as physical activity, dietary patterns, and sleep habits. They can also serve as reminders for medication intake, mindfulness practices, regular checkups, and cancer screenings. [15]
The emergence of precision medicine has created extensive opportunities for advancements in modern healthcare and has brought practical significance to the concept of personalized medicine. Precision medicine is revolutionizing disease classification by establishing a personalized system that deviates from the conventional approach. Precision medicine plays a crucial role in precisely categorizing and diagnosing diseases by integrating patients' clinical characteristics with diverse omics data.
This approach enables the implementation of targeted prevention and treatment strategies, ensuring that patients receive the appropriate interventions, dosages, and timing tailored to their specific needs. [16]
Let us explore the significance of precision and personalized medicine in the context of various diseases.
(a) Cancer
Oncology has undoubtedly been a pioneer in precision medicine. The shift towards personalized therapies is likely driven by several factors, including the prevalent cytotoxicity and significant side effects linked with current "one size fits all" cancer medications. Additionally, the identification of specific vulnerabilities in tumors as potential therapeutic targets further supports the adoption of personalized treatment approaches. Notably, there are two main ways through which therapies can be created to more specifically target cancer cells:
Selectively disrupting the pathways required for cancer cell survival or growth (pathway-based targeted therapy)
Manipulating patients' immune systems in order to trigger an immune response against cancer cells (immunotherapy)
Targeted treatments protect healthy cells and encourage the substratification of types of tumor, enabling the customization of treatments in accordance. [17] Individuals carrying specific variations in the BRCA1 or BRCA2 genes have a lifetime risk of up to 85% to develop breast cancer and up to 60% to develop ovarian cancer. The BRCA1 and BRCA2 genetic tests can provide valuable guidance for implementing preventive measures, including more frequent mammography screenings, prophylactic surgeries, and the consideration of chemoprevention strategies. [18]
Imatinib, an inhibitor that specifically targets the BCR-ABL fusion gene in chronic myelogenous leukemia and gain-of-function mutations in the genes responsible for mast/stem cell growth factor receptor (KIT) or platelet-derived growth factor receptor-α (PDGFRα) in gastrointestinal stromal tumors, stands as an early and notable example of successful targeted cancer therapy. [17]
(b) Asthma
In the realm of chronic inflammatory diseases like asthma, the pursuit of precision medicine and personalized therapy represents significant goals. To accomplish this, it is essential to accurately classify the various subtypes of asthma using reliable diagnostic criteria that incorporate genetic markers and biomarkers. [19] For instance, despite drastically lowering eosinophil levels, mepolizumab (an interleukin-5 [IL-5] antibody) was shown to be clinically ineffective in those with moderate asthma. Around 10 years later, it was demonstrated to be incredibly effective in the subset of people with hypereosinophilic syndrome.
Since the IL-5 eosinophil route is less relevant in the majority of asthmatics, it was anticipated that blocking it wouldn't have any clinically meaningful impact. According to research, free Immunoglobulin E (IgE) levels must be below 50 g/mL for Omalizumab to be effective. Its dose is adjusted for body weight and baseline IgE in order to achieve the desired reduction in IgE levels. [17]
(c) Rare diseases
Precision medicine paves the way to identify potential therapies for individuals with rare diseases, considering that approximately 1 in 10 people are affected by one of the 10,000 rare diseases. [20] Individuals with rare diseases often experience the challenging journey known as the diagnostic odyssey. This entails enduring long and exhaustive cycles of tests and clinical visits, sometimes spanning several years, in the hope of identifying the underlying cause of their condition. For such people, obtaining a genetic diagnosis marks the termination of the diagnostic odyssey and signifies the commencement of a therapeutic odyssey. [21]
(d) Metabolic disorders
(i) Dyslipidemia: The creation of proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors is a clear example of how molecular, phenotypic, and genetic data are used to support the pursuit of PCSK9 as a therapeutic target for hypercholesterolemia. Scientific evidence has confirmed that PCSK9, a protein secreted by the liver, circulates in the bloodstream and binds to low-density lipoprotein (LDL) receptors, which play a crucial role in the removal of cholesterol from circulation. This binding then causes LDL receptor endocytosis and subsequent degradation.
By increasing the number of LDL receptors that are accessible as a result of PCSK9 inhibition, plasma LDL-C levels are decreased. Following the administration of alirocumab and evolocumab, a considerable decrease (36–60 %) in LDL-C was seen, which led to their US FDA approval. The ANGPTL4 gene's loss of function mutation is linked to healthy lipid profiles and a decreased risk of coronary artery disease. These effects of monoclonal antibodies are supported by animal models, which strengthens the case for ANGPTL4 as a potential therapeutic target for coronary artery disease. [17]
(ii) Diabetes Mellitus:
In diabetes, personalized medicine encompasses various aspects, including the identification of risk factors, allocation of resources, selection of tailored therapies, and monitoring response through biomarkers. Genetic variations, such as single nucleotide polymorphisms (SNPs) in genes like ABCC8, SLC22A1, SLC22A2, and PPARG, influence the response to oral anti-diabetic drugs. Personalized medicine in diabetes extends beyond addressing clinical and laboratory abnormalities and considers the psychological and social well-being of individuals with diabetes.
Additionally, the integration of digital health initiatives and computational platforms with omics data (genomics, proteomics, metabolomics, and transcriptomics) has revolutionized personalized medicine in diabetes care. It enables more precise drug prescribing, minimizing the need for trial and error, and reducing the time wasted on ineffective responses or with adverse effects. [22]
(e) Neurodegenerative disorder
Within the field of neurology, precision medicine has the potential to offer screening options, implement timely detection and diagnosis techniques, and customize treatment plans based on an individual's unique clinical, genetic, biological traits, and risk factors. [23] With the development of patient-specific precision-targeted personalized therapies, next-generation diagnostics, neuroimaging modalities, and novel neurodegenerative disease models, it will be possible to effectively treat neurodegenerative disorders like amyotrophic lateral sclerosis, frontotemporal dementia, Huntington's disease, Parkinson's disease, and Alzheimer's disease. [24]
(f) COVID-19
The emergence of the COVID-19 pandemic offers a unique chance to leverage the benefits of personalized medicine in addressing a novel public health challenge, encompassing prevention, diagnosis, treatment, surveillance, and overall management. [25] With unlimited resources, a precision medicine strategy would start by studying the genomes of a large group of individuals who have already been exposed to SARS-CoV-2 but are asymptomatic, as well as a similar-sized group of individuals with known risk factors who are either dying from the disease or are in critical condition. [26]
Personalized medicine can play a pivotal role in understanding an individual's susceptibility to infection and the variability in clinical outcomes, prognosis, and response to treatment. The incorporation of personalized medicine into clinical practice holds immense potential for transforming healthcare by facilitating the creation of preventive and therapeutic approaches that are specifically customized to individual profiles. This approach can enhance the detection of outbreaks and the identification of transmission patterns at a more localized level.
The combination of SARS-CoV2 genome sequencing and the assessment of specific genetic variants in patients can provide valuable insights to inform clinical decision-making and improve our fight against the outbreak. Furthermore, it can facilitate the effective stratification and selection of patients for clinical trials, thereby boosting the chances of procuring positive outcomes. [25]
Benefits and Challenges

Precision and personalized medicine offer transformative potential in healthcare, but they also bring forth a range of benefits and challenges that need to be understood and addressed.
Benefits
1. Targeted Treatment: One of the key advantages of precision medicine and personalized medicine is the ability to deliver targeted treatments based on a patient's specific genetic or molecular profile. This approach allows for more effective treatments with reduced side effects, as therapies are tailored to the specific characteristics of an individual's disease.
2. Improved Diagnosis: Precision medicine and personalized medicine utilize advanced diagnostic tools and techniques to identify diseases at an early stage and with greater accuracy. This early and precise diagnosis can result in timely interventions, thus boosting the chances of successful outcomes.
3. Predictive Risk Assessment: By analyzing an individual's genetic and environmental data, precision medicine and personalized medicine can help assess a person's risk of developing certain diseases. This knowledge enables proactive measures, such as lifestyle modifications or preventive interventions, to mitigate or delay disease onset.
4. Enhanced Drug Development: These approaches facilitate the identification of specific molecular targets for drug development, leading to the design of more effective therapies. By understanding the underlying mechanisms of diseases at a molecular level, researchers can develop drugs that selectively target disease-causing factors, improving treatment outcomes.
5. Patient Engagement and Empowerment: Precision medicine and personalized medicine empower patients by involving them in their own healthcare decisions. By understanding their unique genetic and environmental factors, patients can actively participate in treatment planning and make informed choices regarding their healthcare. [12, 13, 27]
Challenges
While personalized and precision medicine is anticipated to yield advancements in numerous areas of healthcare, there are still many obstacles hindering its application in clinical practice. [6]
1. Data Integration and Privacy: The successful implementation of precision medicine and personalized medicine relies on the integration and analysis of large amounts of patient data, including genetic, clinical, and lifestyle information. Ensuring data privacy and security while enabling effective data sharing and analysis poses significant challenges. [28]
2. Cost and Accessibility: Implementing precision medicine and personalized medicine approaches can be expensive, particularly when considering the need for advanced genomic testing, data analysis, and tailored treatment options. The cost-effectiveness and accessibility of these approaches need to be carefully evaluated to ensure equitable access to personalized healthcare. [29]
3. Ethical and Legal Considerations: The use of genetic and molecular information in precision medicine raises ethical and legal concerns, such as privacy, consent, and potential discrimination based on genetic characteristics. Adequate guidelines and regulations must be in place to address these issues and protect patient rights. [30]
4. Limited Evidence Base: While precision medicine and personalized medicine hold great promise, the evidence base for their effectiveness in various diseases is still evolving. Further research and clinical trials are necessary to establish the validity and efficacy of these approaches across different populations and disease contexts. [31]
5. Implementation Challenges: Integrating precision medicine and personalized medicine into routine clinical practice requires significant changes in healthcare delivery systems, including training healthcare providers, developing appropriate infrastructure, and incorporating new technologies. Overcoming these implementation challenges is essential for the widespread adoption and successful integration of these approaches. [32]
Take Away!
Gone are the days of one-size-fits-all treatments; instead, healthcare providers now have the tools and knowledge to tailor medical interventions to individual patients based on their unique characteristics and requirements. This paradigm shift has opened up a world of possibilities, allowing for more accurate diagnosis, targeted therapies, and better patient outcomes. [6] Precision and personalized medicine have recently gained popularity across a variety of scientific disciplines, and it is likely to gain significance in the coming years. [10]
As they continue to advance, it brings us closer to a future of healthcare that is tailored to each individual patient, offering more precise, predictable, and potent treatment options. Our expanding knowledge of genetics and genomics, and their influence on health, disease, and drug responses, empowers doctors to enhance disease prevention, deliver more accurate diagnoses, prescribe safer medications, and administer more effective treatments for a wide range of health conditions that impact our well-being. [33]
The rise of high-throughput technology and biological system development may account for the substantial interest in this field. Advancements in the interpretation and utilization of genetic data will contribute to a deeper comprehension of physiological processes in both healthy and diseased states. This enhanced knowledge will facilitate personalized approaches to treatment and diagnosis. Additionally, personalized medicine strives to save healthcare expenses and avoid side effects by making it easier to choose the appropriate medication at the correct time for a given patient. But, personalization cannot be applied to all disorders.
While making decisions, different illnesses must integrate non-biological, biological, and environmental aspects. Additionally, it is still necessary to assess the importance of each personalized treatment strategy. In order to validate the efficacy of any proposed personalized approach, it is essential to conduct clinical trials that can provide evidence of its superiority over existing guideline-based therapies. [10]
In conclusion, precision medicine and personalized medicine have transformative potential in healthcare. By leveraging individual variability and tailoring interventions to specific patient needs, these approaches offer more precise diagnoses, targeted therapies, and improved patient outcomes. Their integration into routine clinical practice has the potential to revolutionize healthcare delivery and improve population health. [34]
References
1. Stefanicka-Wojtas D, Kurpas D. Personalised Medicine-Implementation to the Healthcare System in Europe (Focus Group Discussions). Journal of Personalized Medicine. 2023 Feb 21;13(3):380.
2. What Are Precision Medicine and Personalized Medicine?
Available from: https://healthitanalytics.com/features/what-are-precision-medicine-and-personalized-medicine [Last accessed on: 31 May 2023]
3. Is Personalized Medicine the Future of Healthcare? Available from: https://www.news-medical.net/health/Is-Personalized-Medicine-the-Future-of-Healthcare.aspx [Last accessed on: 31 May 2023]
4. Prosperi M, Min JS, Bian J, Modave F. Big data hurdles in precision medicine and precision public health. BMC Medical Informatics and Decision Making. 2018 Dec 29;18(1):139.
5. Ginsburg GS, Phillips KA. Precision Medicine: From Science To Value. Health Affairs (Millwood). 2018 May;37(5):694-701.
6. Iriart JA. Precision medicine/personalized medicine: a critical analysis of movements in the transformation of biomedicine in the early 21st century. Cadernos de Saúde Pública. 2019 Mar 25;35.
7. Precision vs. Personalized Medicine. Available from: https://www.news-medical.net/health/Precision-vs-Personalized-Medicine.aspx [Last accessed on: 31 May 2023]
8. Johnson KB, Wei WQ, Weeraratne D, Frisse ME, Misulis K, Rhee K, Zhao J, Snowdon JL. Precision Medicine, AI, and the Future of Personalized Health Care. Clinical and Translational Science. 2021 Jan;14(1):86-93.
9. The Shift From Personalized Medicine to Precision Medicine and Precision Public Health: Words Matter! Available from: https://blogs.cdc.gov/genomics/2016/04/21/shift/
[Last accessed on: 31 May 2023]
10. Strianese O, Rizzo F, Ciccarelli M, Galasso G, D’Agostino Y, Salvati A et al. Precision and personalized medicine: how genomic approach improves the management of cardiovascular and neurodegenerative disease. Genes. 2020 Jul 6;11(7):747.
11. Naithani N, Sinha S, Misra P, Vasudevan B, Sahu R. Precision medicine: Concept and tools. Medical Journal Armed Forces India. 2021 Jul;77(3):249-257.
12. National Research Council (US) Committee on A Framework for Developing a New Taxonomy of Disease. Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease. Washington (DC): National Academies Press (US); 2011.Available from: https://www.ncbi. Bookshelf ID: NBK91503, PMID: 22536618.
13. Collins FS, Varmus H. A new initiative on precision medicine. The New England Journal of Medicine. 2015 Feb 26;372(9):793-5.
14. Carbonara K, MacNeil AJ, O’Leary DD, Coorssen JR. Profit versus Quality: The Enigma of Scientific Wellness. Journal of Personalized Medicine. 2022 Jan 3;12(1):34.
15. Precision health: Improving health for each of us and all of us. Available from: https://www.cdc.gov/genomics/about/precision_med.htm#:~:text=Precision%20medicine%2C%20also%20called%20personalized,will%20work%20best%20for%20you. [Last accessed on: 30 May 2023]
16. Yuan B. What Personalized Medicine Humans Need and Way to It --also on the Practical Significance and Scientific Limitations of Precision Medicine. Pharmacogenomics and Personalized Medicine. 2022 Nov 2;15:927-942.
17. Akhoon N. Precision medicine: a new paradigm in therapeutics. International Journal of Preventive Medicine. 2021;12.
18. 5 Benefits of Precision Medicine. Available from: https://www.reprocell.com/blog/5-benefits-of-pm [Last accessed on: 30 May 2023]
19. Roth M, Stolz D. Biomarkers and personalised medicine for asthma. European Respiratory Journal. 2019 Jan 1;53(1).
20. Might M, Crouse AB. Why rare disease needs precision medicine-and precision medicine needs rare disease. Cell Reports Medicine. 2022 Feb 15;3(2):100530.
21. Villalón-García I, Álvarez-Córdoba M, Suárez-Rivero JM, Povea-Cabello S, Talaverón-Rey M, Suárez-Carrillo A et al. Precision medicine in rare diseases. Diseases. 2020 Nov 13;8(4):42.
22. Mohan V, Das AK, Mukherjee JJ, Seshadri K, Sujeet J, Sanjay K. From Individualized to personalized medicine in diabetes: an expert overview. Journal of the Association of the Physicians of India. 2019:78.
23. Hampel H, Gao P, Cummings J, Toschi N, Thompson PM, Hu Y et al. The foundation and architecture of precision medicine in neurology and psychiatry. Trends in Neurosciences. 2023 Jan 13.
24. Raikwar SP, Kikkeri NS, Sakuru R, Saeed D, Zahoor H, Premkumar K et al. Next generation precision medicine: CRISPR-mediated genome editing for the treatment of neurodegenerative disorders. Journal of Neuroimmune Pharmacology. 2019 Dec;14(4):608-41.
25. Dopazo J, Maya-Miles D, García F, Lorusso N, Calleja MÁ, Pareja MJ et al. Implementing Personalized Medicine in COVID-19 in Andalusia: An Opportunity to Transform the Healthcare System. Journal of Personalized Medicine. 2021 May 26;11(6):475.
26. How to use precision medicine to personalize COVID-19 treatment according to the patient’s genes. Available from: https://theconversation.com/how-to-use-precision-medicine-to-personalize-covid-19-treatment-according-to-the-patients-genes-142142 [Last accessed on: 30 May 2023]
27. Ashley EA. The precision medicine initiative: a new national effort. JAMA. 2015 Jun 2;313(21):2119-20.
28. Hassan M, Awan FM, Naz A, deAndrés-Galiana EJ, Alvarez O, Cernea A et al. Innovations in Genomics and Big Data Analytics for Personalized Medicine and Health Care: A Review. The International Journal of Molecular Sciences. 2022 Apr 22;23(9):4645
Will Personalized Medicine Mean Higher Costs for Consumers? Available from: https://hbr.org/2018/03/will-personalized-medicine-mean-higher-costs-for-consumers [Last accessed on: 30 May 2023]
30. Cordeiro JV. Ethical and legal challenges of personalized medicine: paradigmatic examples of research, prevention, diagnosis and treatment. Revista Portuguesa de Saúde Pública. 2014 Jul 1;32(2):164-80.
31. Beckmann JS, Lew D. Reconciling evidence-based medicine and precision medicine in the era of big data: challenges and opportunities. Genome medicine. 2016 Dec;8:1-1.
32. Naithani N, Atal AT, Tilak TVSVGK, Vasudevan B, Misra P, Sinha S. Precision medicine: Uses and challenges. Medical Journal Armed Forces India. 2021 Jul;77(3):258-265.
33. WHAT IS PERSONALIZED MEDICINE? Available from: https://www.jax.org/personalized-medicine/precision-medicine-and-you/what-is-precision-medicine#:~:text=Tailoring%20health%20care%20to%20each,personalized%20medicine%20or%20genomic%20medicine.
[Last accessed on: 31 May 2023]
34. Mathur S, Sutton J. Personalized medicine could transform healthcare. Biomedical Reports. 2017 Jul;7(1):3-5.
Comments (1)