Categories
Change Password!
Reset Password!


Human papillomavirus (HPV)-based cervical screening is a globally endorsed strategy for cervical cancer prevention.
While HPV-based screening provides a better shield against invasive cervical cancer risk than cytology-based screening, it also leads to more colposcopy referrals.
Human papillomavirus (HPV)-based cervical screening is a globally endorsed strategy for cervical cancer prevention. While randomized clinical trials (RCTs) have established its superiority over cytology, real-world evidence is pivotal for shaping public health policies.
The goal of this study was to assess the effectiveness of HPV-based versus cytology-based cervical screening in minimizing the risk of invasive cervical cancer after two full screening rounds, using data from a preplanned secondary analysis of a randomized health-care policy trial in Sweden.
Sweden’s capital-region cervical screening program invited women (aged 30–64 years) to take part in a randomized trial comparing HPV-based and cytology-based screening. From 2014 to 2016, 395,725 eligible volunteers were randomly allocated (non-concealed) to either method, with invasive cervical cancer incidence tracked over 8 years. Analyses were conducted on an intention-to-screen basis (all invited women) and per-protocol (those who attended baseline screening as per protocol).
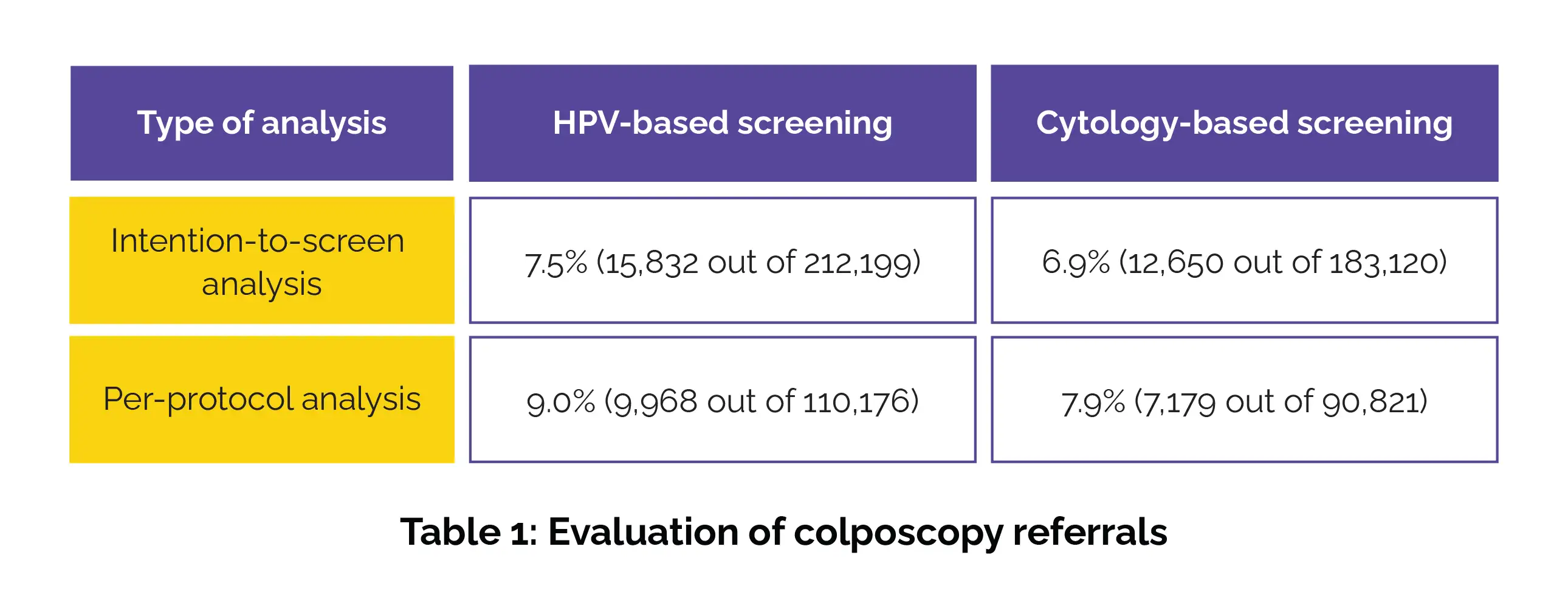
Those invited to HPV-based screening exhibited a 17% lower risk of invasive cervical cancer than those invited to cytology-based screening (hazard ratio [HR] 0.83). Among those who attended screening, HPV-based screening was linked to a 28% lower risk compared to cytology-based screening (HR 0.72). However, HPV-based screening resulted in more colposcopy referrals than cytology-based screening (Table 1).
Women testing HPV-negative at baseline had an invasive cervical cancer risk of 1.3 per 100,000 person-years, whereas those with normal cytology had a higher risk of 9.1 per 100,000 person-years. Women who tested positive for HPV but had a negative cytology triage faced an invasive cervical cancer risk of 79.2 per 100,000 person-years. This risk escalated markedly to 318.2 per 100,000 person-years among those specifically positive for HPV 16 or HPV 18 despite a negative cytology triage.
In a real-world setting, HPV-based screening proved more beneficial in preventing invasive cervical cancer. A single negative HPV test at baseline was linked with an exceptionally low risk over 8 years. However, HPV positivity despite a negative cytology triage signaled a substantial cancer risk, underscoring the need for tailored follow-up strategies.
The Lancet Public Health
Human papillomavirus-based cervical screening and long-term cervical cancer risk: a randomised health-care policy trial in Sweden
Jiangrong Wang et al.
Comments (0)