Categories
Change Password!
Reset Password!


Postoperative visceral pain is often a challenging complication following endoscopic retrograde cholangiopancreatography (ERCP).
Compared to fentanyl, oxycodone provides superior pain relief, lower inflammatory cytokines, and fewer instances of postoperative vomiting in children undergoing ERCP.
Postoperative visceral pain is often a challenging complication following endoscopic retrograde cholangiopancreatography (ERCP). This randomized, double-blind study explored the effectiveness of oxycodone versus fentanyl in tackling pain and inflammation in pediatric patients undergoing ERCP.
Overall, 82 children (aged 2–18 years) scheduled for elective ERCP were assigned to get either oxycodone (0.2 mg/kg) or fentanyl (2 μg/kg). Pain was assessed at 10, 20, and 30 minutes in the post-anesthesia care unit, and at 6 and 24 hours post-procedure on the ward. Inflammatory cytokines, including interleukin (IL)-6, IL-10, and tumor necrosis factor-alpha (TNF-α) were estimated at baseline, 6 hours, and 24 hours after ERCP.
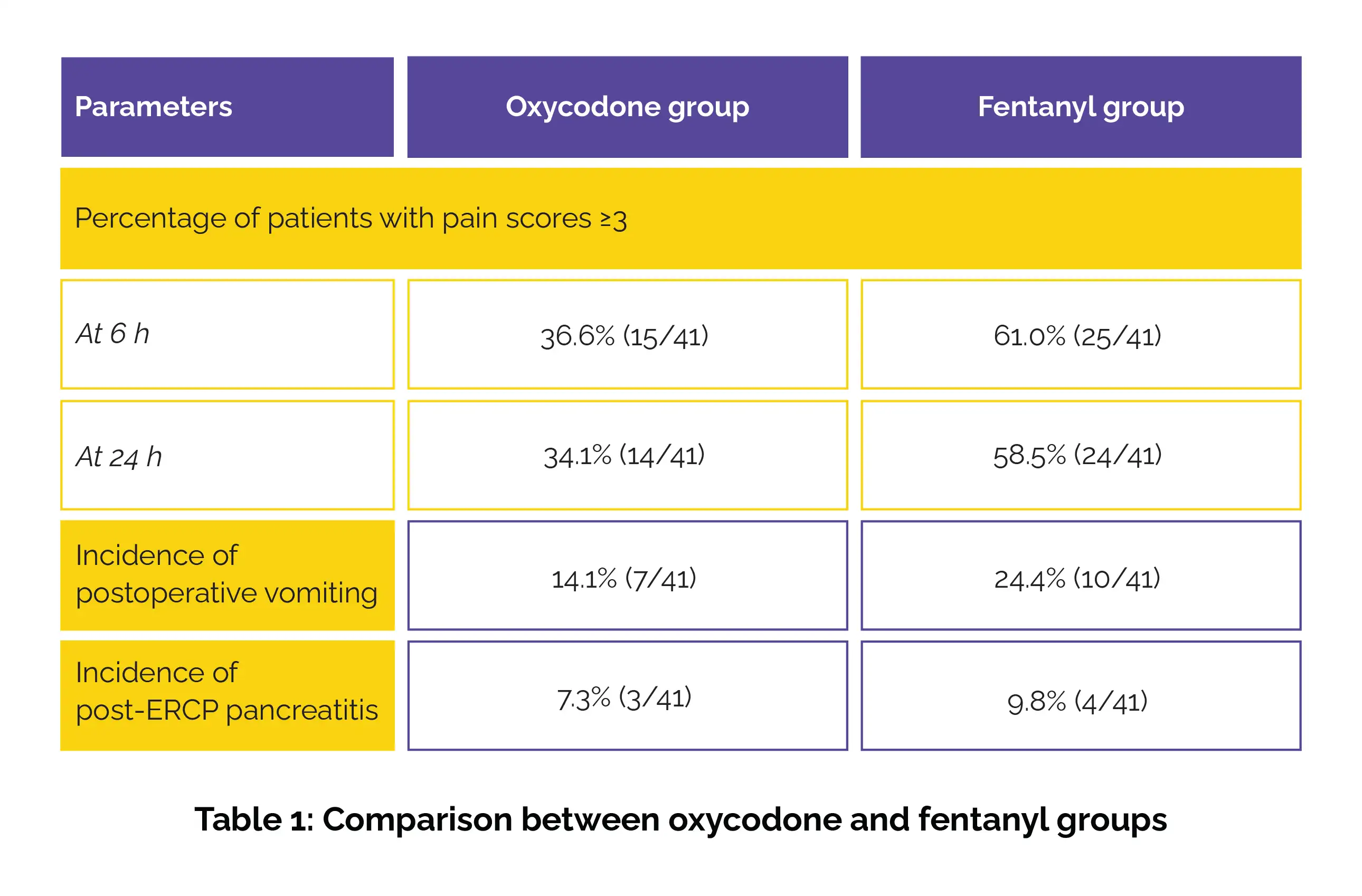
Participants receiving oxycodone experienced lower pain scores at 30 minutes, 6 hours, and 24 hours after ERCP compared to those receiving fentanyl. At 10 and 20 minutes, pain scores were comparable between the groups. Additionally, fewer children in the oxycodone group exhibited pain scores of 3 or higher at 6 and 24 hours after the procedure. The occurrence of postoperative vomiting was lower among those treated with oxycodone. On the other hand, the incidence of post-ERCP pancreatitis was similar across the groups, as shown in Table 1:
Additionally, the oxycodone group exhibited lower levels of inflammatory markers (IL-6 at 6 hours and TNF-α at 24 hours).
Oxycodone (0.2 mg/kg) provides reliable pain control and stable hemodynamics in pediatric patients undergoing ERCP, which may be attributed to its ability to reduce inflammation following the procedure.
Frontiers in Pharmacology
Oxycodone for analgesia in children undergoing endoscopic retrograde cholangiopancreatography: a randomized, double-blind, parallel study
Wei Ji et al.
Comments (0)