Categories
Change Password!
Reset Password!


A 29-year-old patient was diagnosed with non-traumatic pleuritic chest pain. Epipericardial fat necrosis was identified as a potential rare differential diagnosis for acute chest pain. The patient experienced symptom relief with nonsteroidal anti-inflammatory therapy.
A 29-year-old patient was diagnosed with non-traumatic pleuritic chest pain. Epipericardial fat necrosis was identified as a potential rare differential diagnosis for acute chest pain. The patient experienced symptom relief with nonsteroidal anti-inflammatory therapy.
A 29-year-old male patient arrived at the emergency department with non-traumatic pleuritic chest pain persisting for six days. The pain was described as sharp, intense, and severe when lying on his back (dorsal decubitus position). Acute pleuritis was the initial hypothesis. To diagnose epipericardial fat necrosis (EFN), the patient underwent a chest computed tomography scan. After the diagnosis, he was released with a medium-term anti-inflammatory treatment plan.
INTRODUCTION
Chest pain is a frequent and potentially life-threatening condition encountered in the emergency department, necessitating prompt investigation and management. EFN is defined as an inflammatory process that takes place in the mediastinal fat around the heart. It is an uncommon, benign source of chest pain in young individuals that can resemble conditions like myocardial infarction, pulmonary embolism, and pericarditis.
Its primary symptom is pleuritic pain, which is commonly described as sharp and localized discomfort in the chest or shoulder area. This pain tends to worsen with coughing, chest movement, and deep breathing. During the physical examination, typical findings may encompass raised heart rate (tachycardia), rapid breathing (tachypnea), and in some cases, the presence of a cardiac friction rub. It is vital to consider potentially serious conditions that may present with similar manifestations, like acute aortic syndrome, acute coronary syndrome, pericarditis, pneumothorax, or pulmonary embolism.
Although the first documented case of EFN in medical literature dates back to 1957, and there have been some reports discussing tomography findings since then, comprehensive guidelines for diagnosing and treating this condition are still lacking. This case report emphasizes an unusual potential cause of pleuritic chest pain: EFN. It presents a case of a patient suffering from acute pleuritic chest pain who sought medical attention at the emergency ward. The purpose of this report is to raise awareness about the possible diagnosis of EFN in individuals at low risk and to examine the existing literature focusing on indicators that aid in a precise diagnostic approach. Furthermore, an algorithm for a diagnostic approach has also been proposed.
MEDICAL HISTORY
NA
Upon admission, the vital signs of the patient were recorded as follows:
Cardiovascular and pulmonary assessments did not indicate any pericardial friction rub or other notable findings. Electrocardiography showed early repolarization. Chest radiography indicated opacity at thorax anterior base, slight blurring of cardiac silhouette, and an elevated left dome of diaphragm. Point-of-care ultrasonography did not reveal any signs of pericarditis or cardiac effusion. The C-reactive protein level was measured at 7.3 mg/L (normal range <5 mg/L). The D-dimer, hemogram, and troponin levels were found to be within the normal range.
This case report presents a typical presentation of EFN in young, healthy individuals experiencing pleuritic acute chest pain. Despite an initial negative work-up for common cardiovascular and pulmonary causes in the emergency department, the diagnosis was not made due to the limited resolution of chest radiography and lack of suspicion for this condition. However, upon readmission and subsequent chest tomography, EFN was identified.
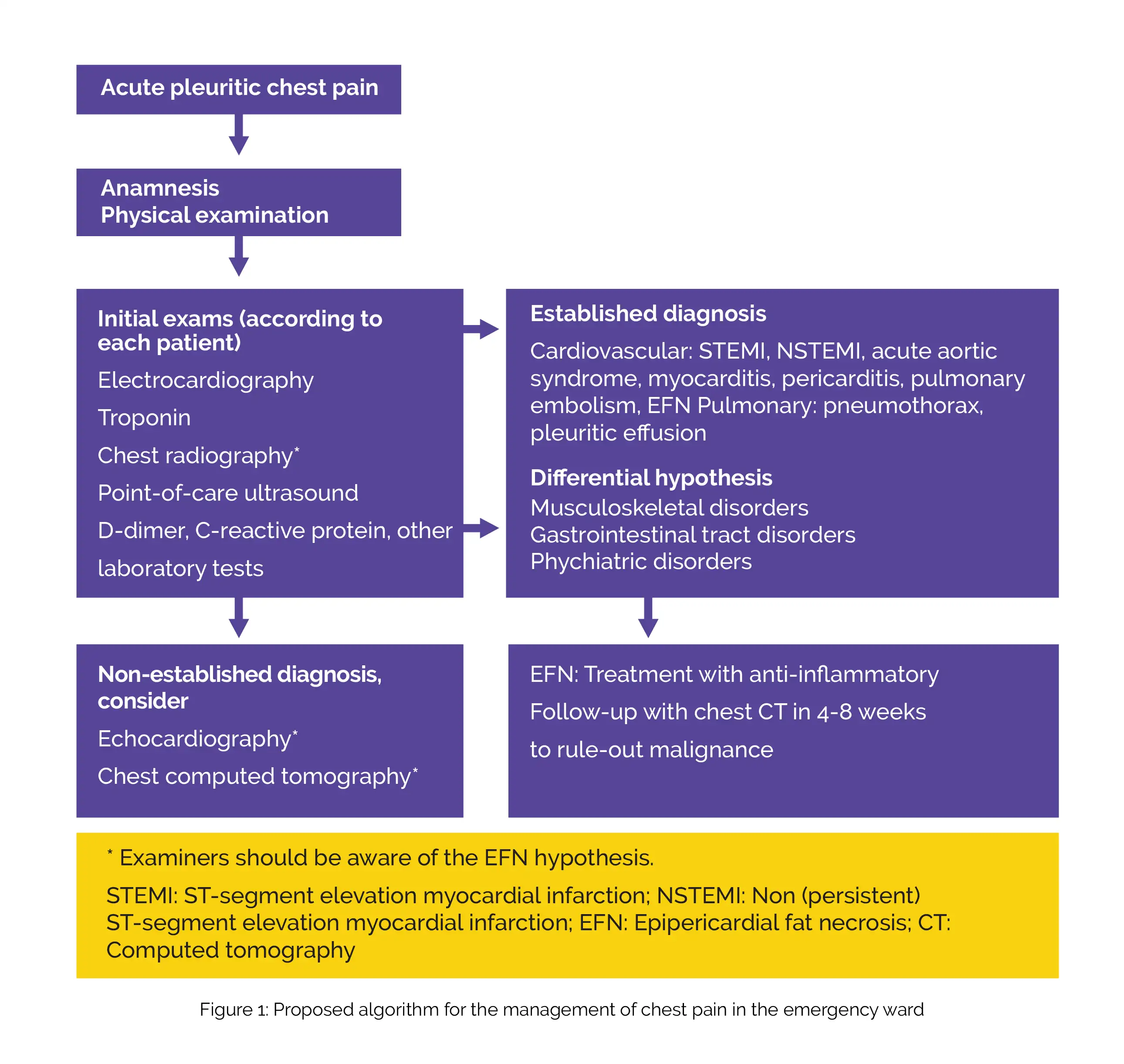
Differential diagnoses for EFN encompass primary fatty tumors (such as thymolipoma, teratoma, liposarcoma, and lipoma), mediastinitis, and diaphragmatic hernias. To facilitate EFN diagnostic process and management, an algorithm for a diagnostic approach was proposed (Figure 1).
The patient's symptoms got better with nonsteroidal anti-inflammatory therapy.
In the United States, non-traumatic acute chest pain accounts for about 8% of all visits to the emergency ward annually. Among these cases, acute coronary syndrome is the primary life-threatening condition and the main reason for initial evaluation. Considering non-cardiovascular causes, musculoskeletal chest pain is the most common etiology, accounting for 44.7% of cases, followed by psychiatric causes (4%), gastrointestinal tract disorders (2.6%), and pulmonary illnesses (2.2%).
However, a significant percentage of individuals (about 46%) are released from medical care with a non-specific diagnosis of chest pain, which includes the possibility of undetermined cardiovascular causes. While it is adequate to discharge many patients early, certain conditions may necessitate additional investigations and specific treatments. EFN commonly manifests as sudden-onset pleuritic chest pain in young individuals who are otherwise healthy. Although it is a harmless and self-resolving condition, it can trigger anxiety, extensive testing to assess severe chest pain, and repeat visits to the emergency department.
The exact cause of EFN remains uncertain; however, the prevailing hypotheses encompass ischemia resulting from spontaneous twisting of the vascular pedicle or rupture of capillaries due to elevated intrathoracic pressure linked with the Valsalva maneuver. Typically, the diagnosis of EFN is incidental, discovered during imaging tests conducted for other suspected pulmonary or cardiac conditions. While there are case reports and some reviews available in the medical literature, this condition remains unfamiliar to many clinicians.
Diagnosis is often fortuitous, and comprehensive guidelines for suspected cases have yet to be proposed in previous studies. Electrocardiogram (ECG) changes are rarely witnessed in cases of EFN, and when present, they are typically nonspecific repolarization findings. Blood tests may indicate a mild rise in the levels of D-dimer, C-reactive protein, and white blood cells. Chest radiography seldom reveals the signs of atelectasis, pleural effusion, paracardiac opacity, or pericardial thickening. EFN has been detected in only 0.26% of radiographs carried out in the emergency department to examine chest pain.
There is limited current research available on the use of point-of-care ultrasound and echocardiography in this particular context. Few researchers have documented the presence of hyperechoic nodules enclosed by a hypoechoic halo within epicardial fat, in conjunction with adjacent hyperechogenic adipose tissue. The definitive method for diagnosing EFN involves detecting pericardial thickening and a well-defined fatty lesion with dense strands using magnetic resonance imaging or computed tomography. According to the findings of a retrospective analysis of 7,463 chest computed tomography scans conducted in the emergency department for chest pain, a 2.15% incidence of EFN, both with and without pleural effusion was reported.
Radiologists must be aware of this possibility, as EFN is frequently misdiagnosed even with these imaging examinations. Treatment typically involves anti-inflammatory agents and follow-up chest computed tomography at four-eight weeks for confirming healing and excluding the presence of tumors. The prognosis for EFN is generally favorable, and there have been no reports of tamponade, chronic pericarditis, recurrence, or chronic pain.
The case report details a specific instance where a patient presented with acute chest pain, which was initially suspected to be a heart-related issue. However, further investigation revealed EFN as the underlying cause. The report emphasizes the importance of considering this condition in the differential diagnosis of acute chest pain, especially when other cardiac causes have been ruled out.
LEARNING
EFN is a rare condition characterized by inflammation and necrosis of the fat tissue surrounding the heart (epipericardial fat). The condition can imitate the symptoms linked with other cardiac disorders, thereby posing diagnostic difficulties. This case serves as an example to remind healthcare professionals to consider the diagnosis of EFN in patients suffering from non-traumatic pleuritic chest pain.
REFERENCES
Einstein (Sao Paulo)
Epipericardial fat necrosis as a differential diagnosis of acute chest pain: a case report and algorithm proposal for diagnostic approach
Tarso Augusto Duenhas Accorsi et al.
Comments (0)