Categories
Change Password!
Reset Password!


This study aimed to explore the link between long-term cumulative blood pressure (cBP) and future cardiovascular outcomes in Chinese adults who had no history of cardiovascular disease (CVD) at baseline.
In middle-aged and older adults, cumulative blood pressure can effectively predict cardiovascular risk profile.
This study aimed to explore the link between long-term cumulative blood pressure (cBP) and future cardiovascular outcomes in Chinese adults who had no history of cardiovascular disease (CVD) at baseline.
Overall, 6,435 volunteers (aged 45 years and above) from the China Health and Retirement Longitudinal Study (CHARLS) were analyzed. cBP was derived as the area under the curve using data from 2011 (Wave 1) to 2013 (Wave 2). Outcomes of interest encompassed incident CVD, heart disease, and stroke.
Over a 5-year median follow-up period, there were 1,101 CVD events, 826 cases of heart disease, and 351 strokes. Each 1-standard deviation rise in cumulative systolic BP (cSBP), cumulative diastolic BP (cDBP), and cumulative mean arterial pressure (cMAP) was linked to a heightened likelihood of CVD, heart disease, and stroke (Table 1).
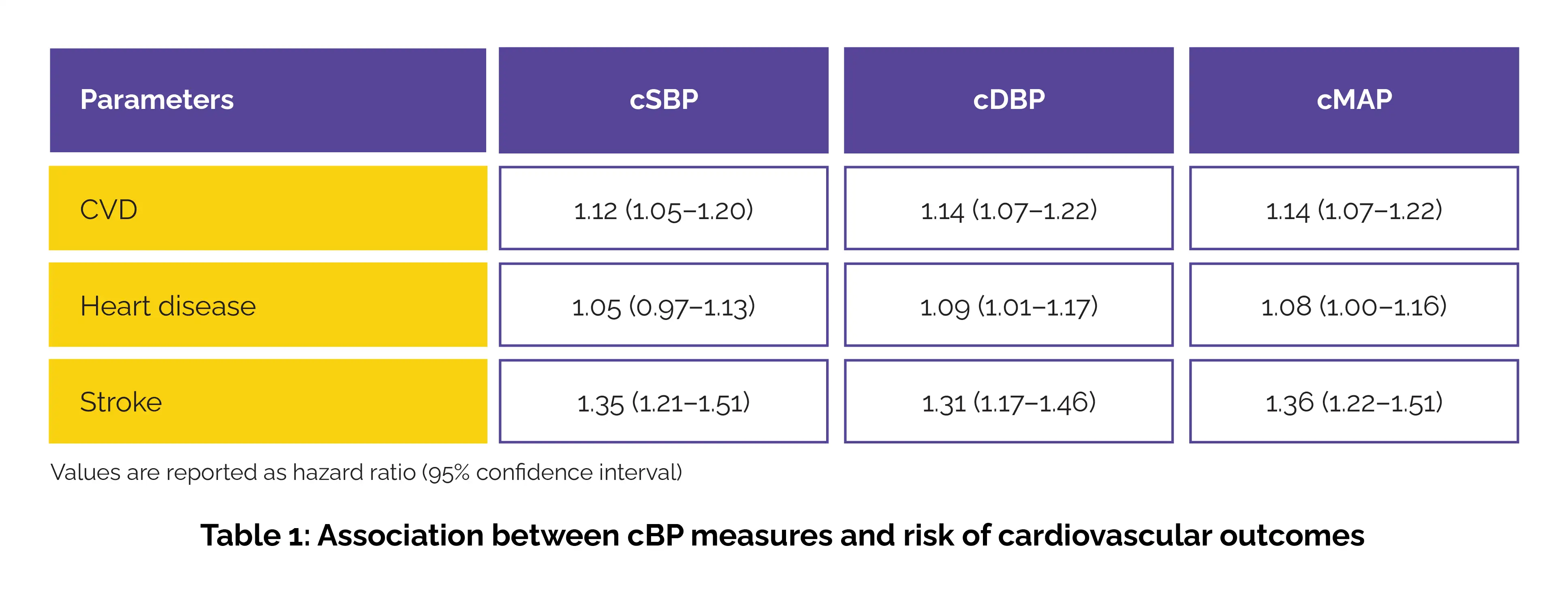
Notably, these associations with CVD were confined to individuals under 60 years of age. Furthermore, cumulative pulse pressure (cPP) showed a prominent link with stroke risk across all ages (hazard ratio: 1.23). No evidence of non-linear associations was witnessed (p-nonlinear > .05). In predictive performance, cumulative BP metrics illustrated superior discriminative power over baseline BP readings (C statistics, p < .001).
Long-term exposure to elevated cSBP, cDBP, and cMAP was linked to greater CVD risk, particularly in those under 60, while cPP was associated with stroke regardless of age. Cumulative BP measures may offer a more reliable predictor of cardiovascular events than single-time BP readings, underscoring the importance of sustained BP control in cardiovascular risk assessment.
Annals of Medicine
Cumulative blood pressure predicts risk of cardiovascular outcomes in middle-aged and older population
Fang-Fei You et al.
Comments (0)